SANTA CLARA, Calif., June 4, 2024 /PRNewswire/ — Zeto, Inc., a privately owned medical technology company, has announced that its innovative next-generation product, named the ONE, has received 510(k) clearance from the U.S. Food and Drug Administration (FDA).
Zeto ONE is approved for EEG Brain Monitoring across hospital, home, ambulance, and air transport environments.

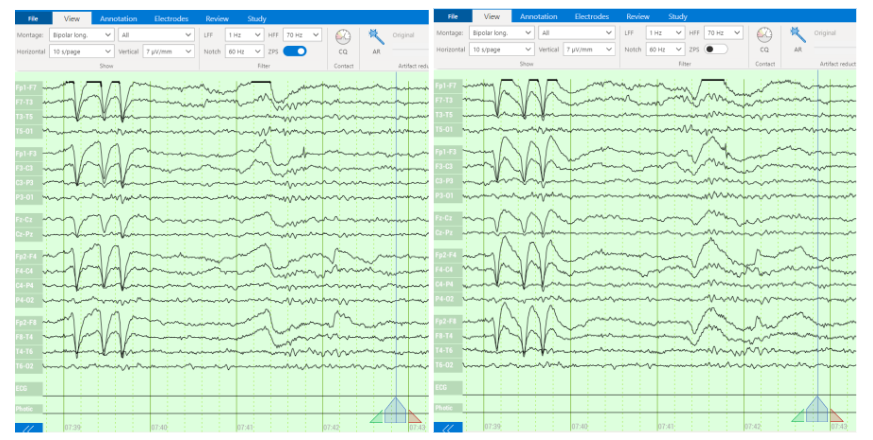
Electroencephalography (EEG) needs in health care remain significantly unmet due to permanent shortage of trained EEG technologists. New EEG products need to be easy to use for any staff, comfortable to the patient and provide excellent signal quality. However, hospitals also require comprehensive full-montage1,2 EEG for thorough coverage of clinically significant events, video capabilities to aid physicians in interpretation, and dependable diagnostic software for neurological emergencies. Without these elements, genuine progress in neurological care will remain unrealized.
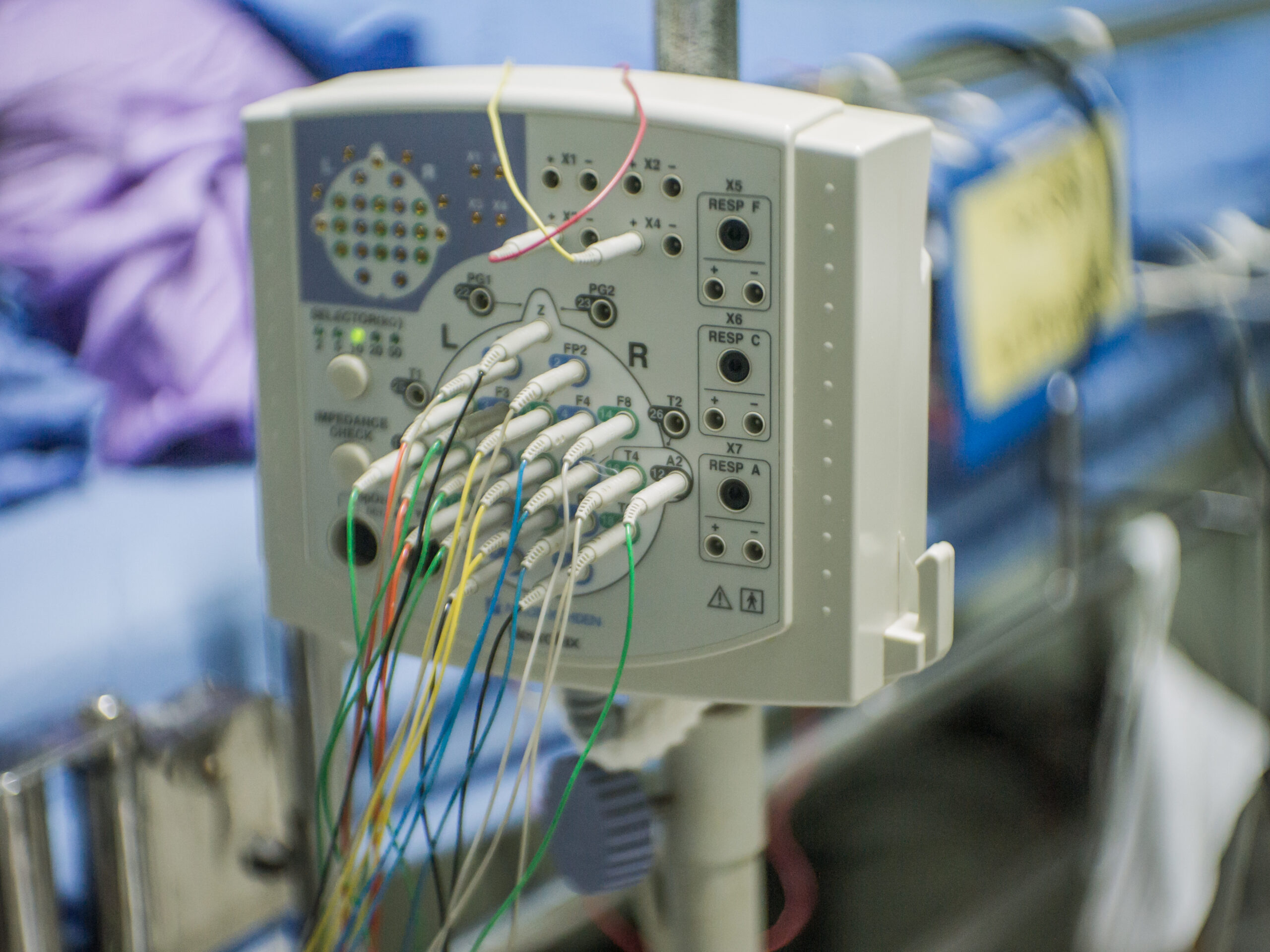
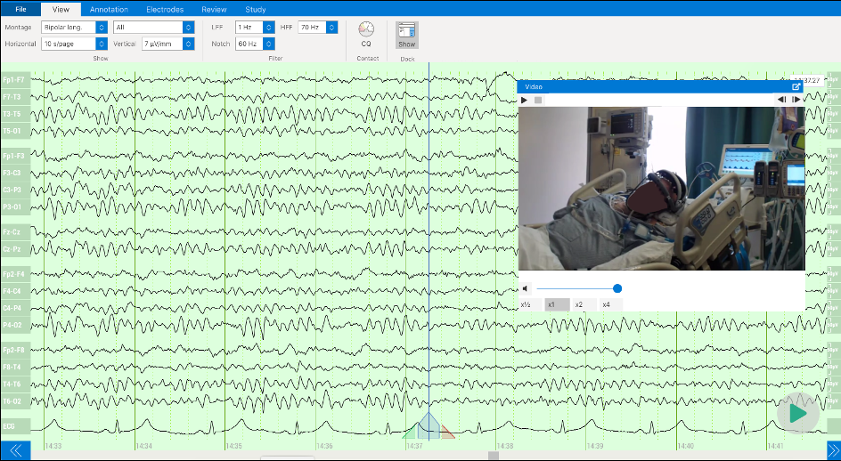
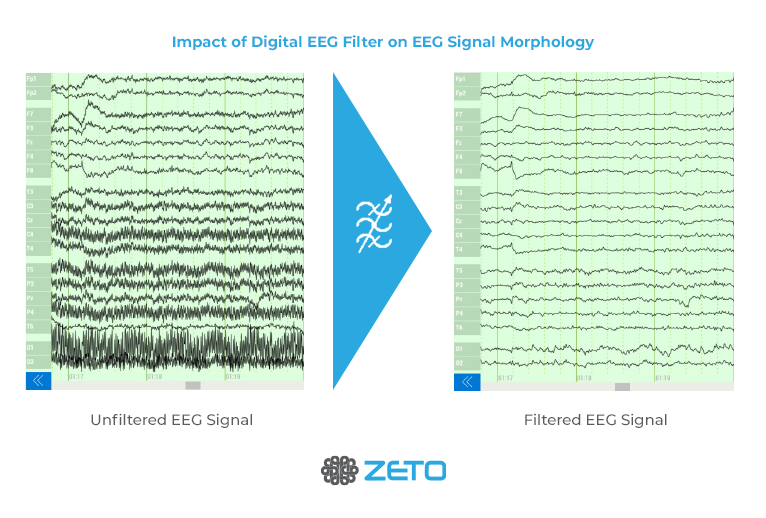
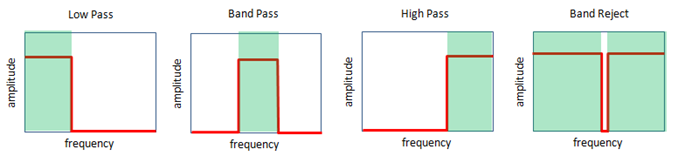
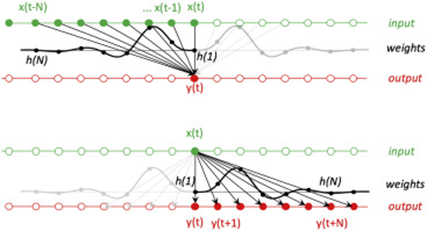
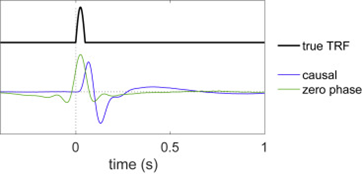
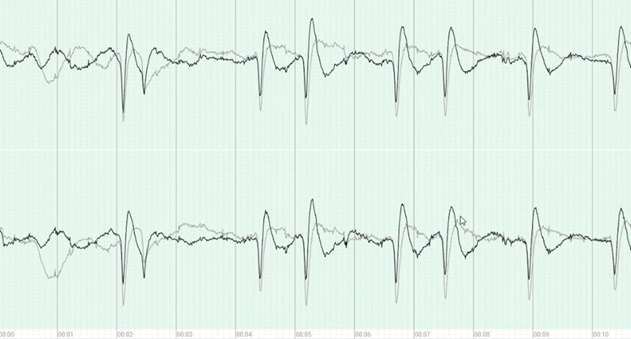
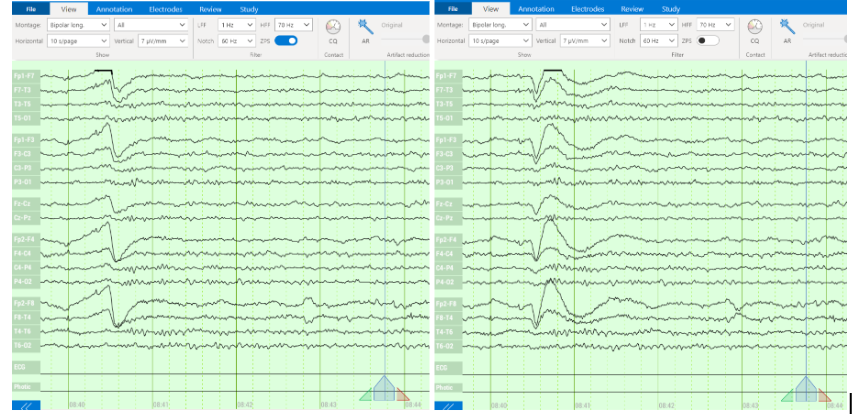
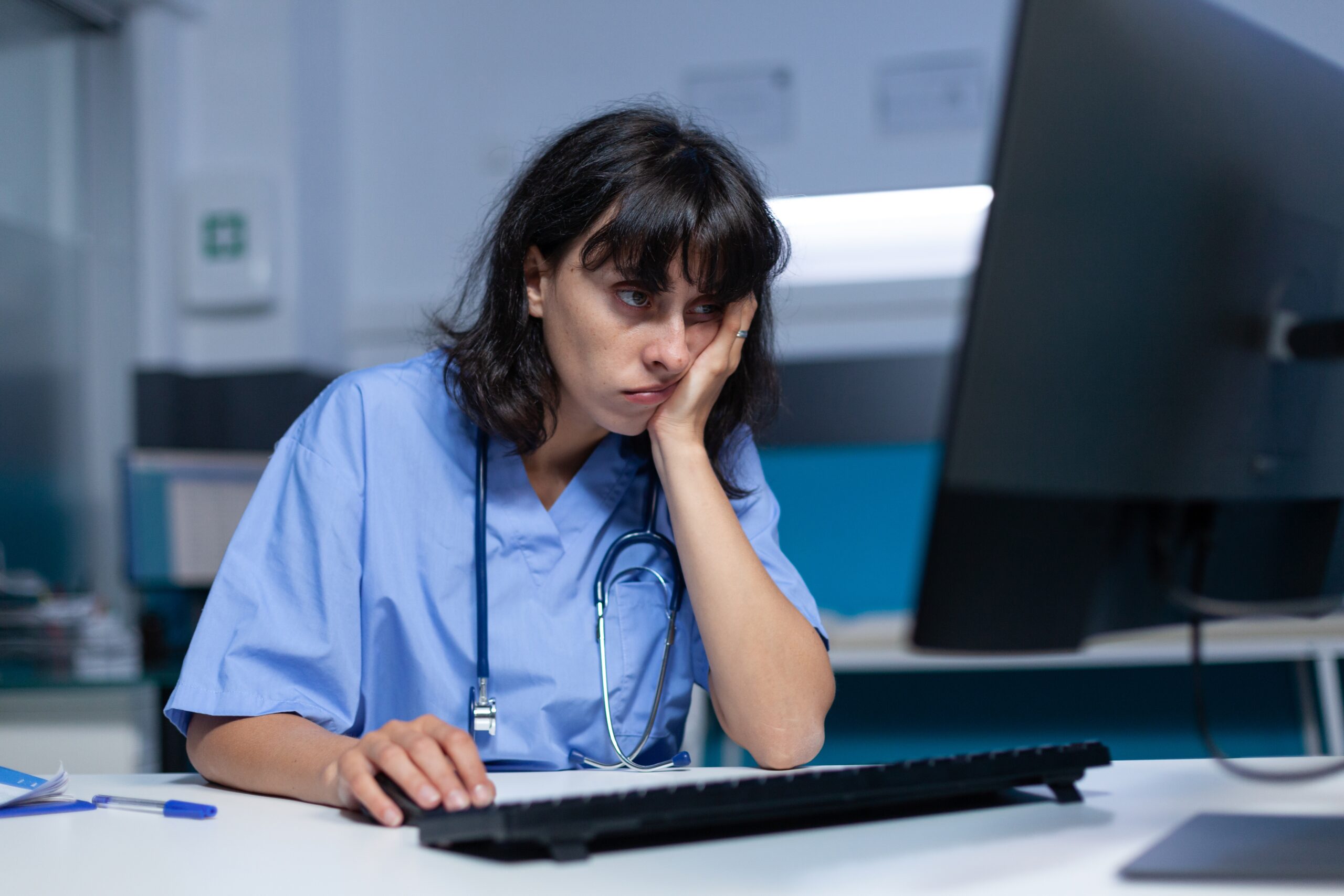
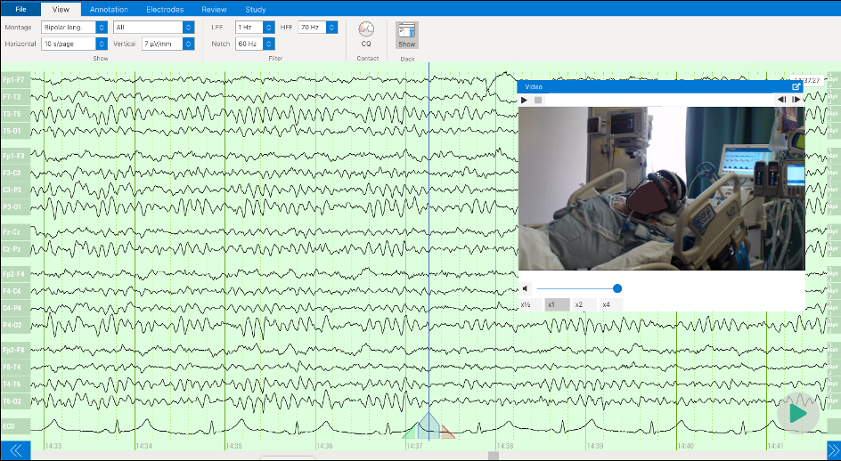
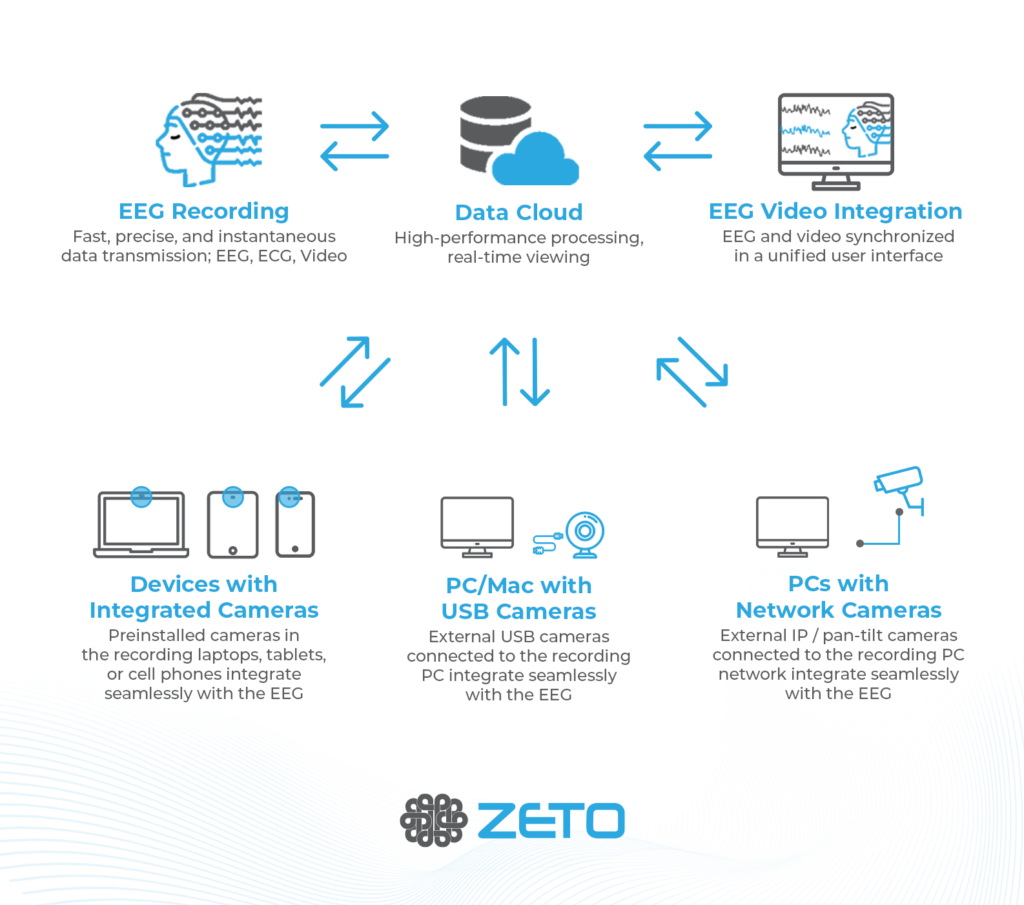
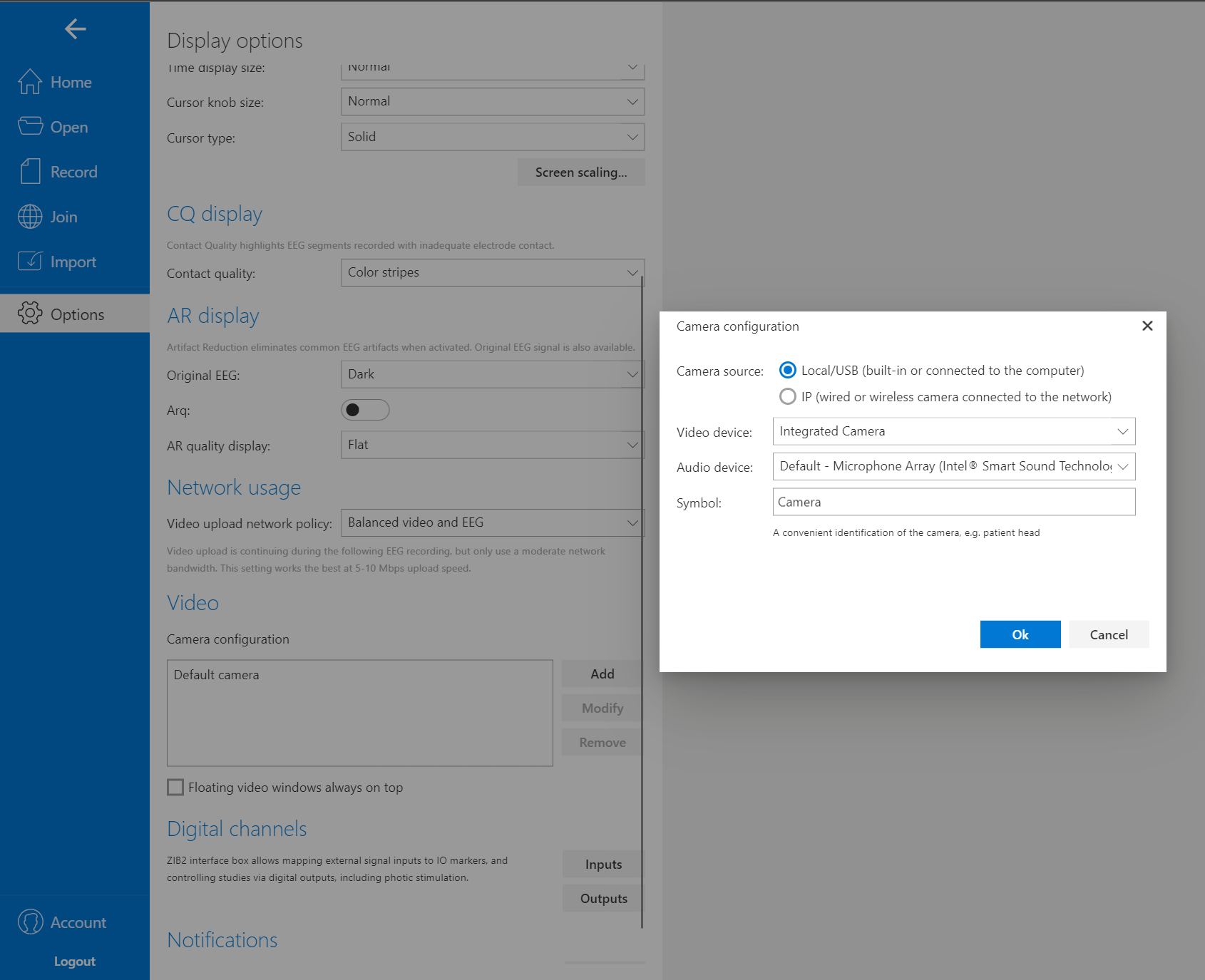
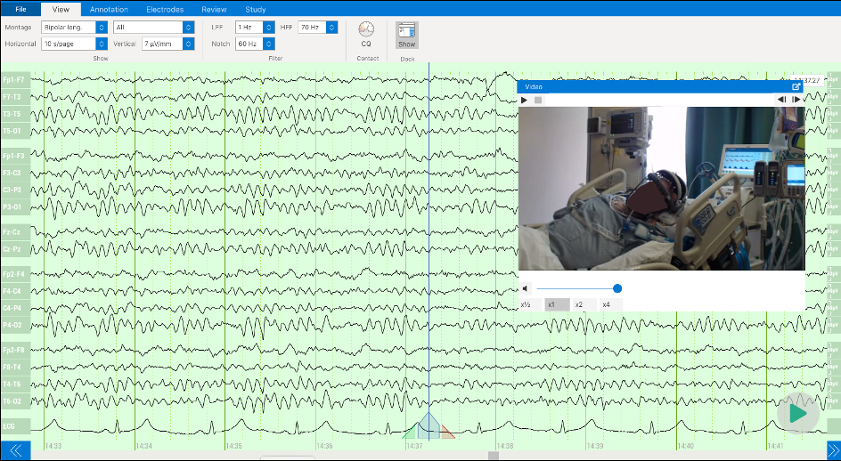
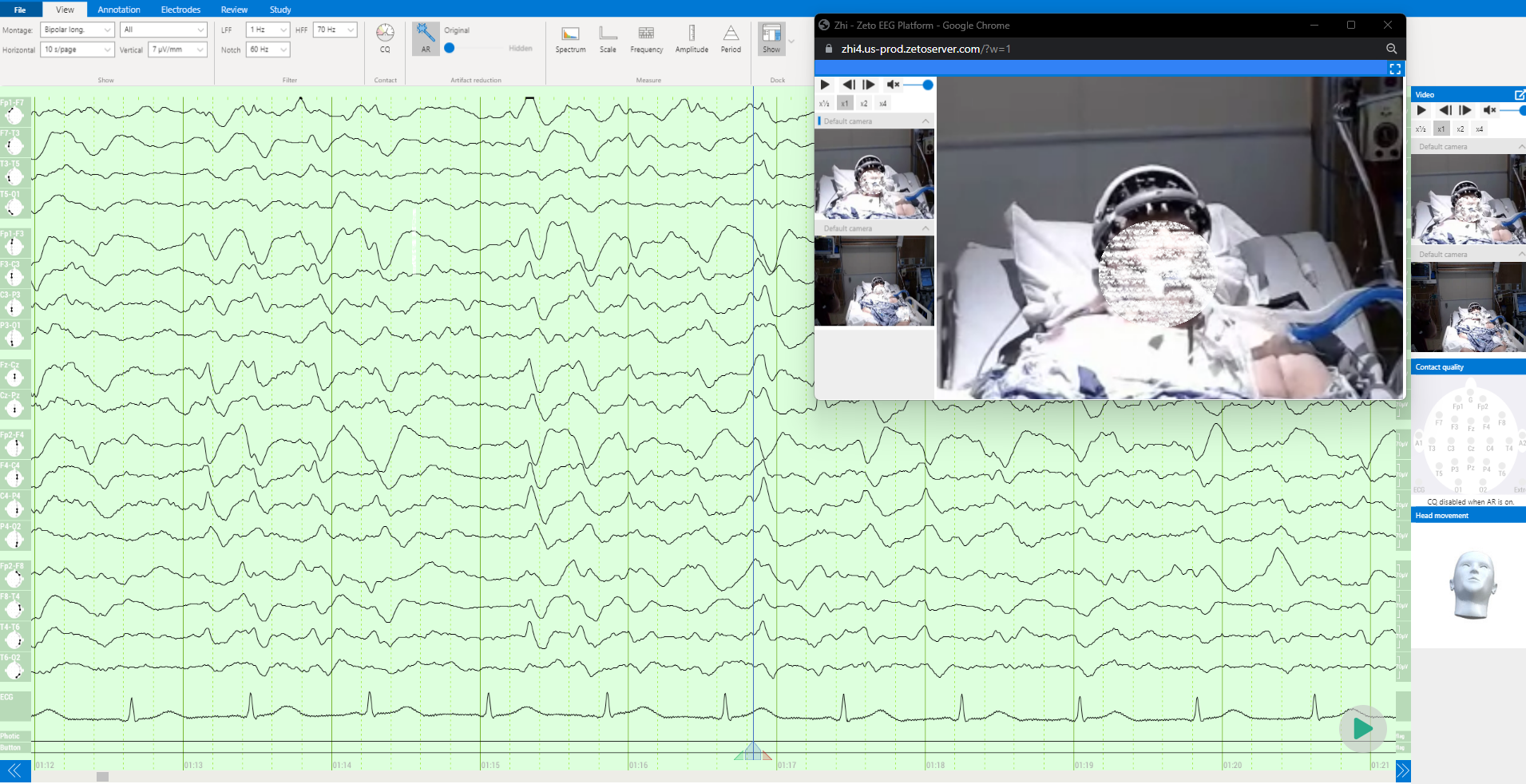
ONE consists of a user-friendly headset equipped with 21 soft-tip electrodes positioned according to the commonly followed 10-20 EEG3 system, accompanied by intuitive LED feedback for easy adjustments. It requires minimal training for any healthcare professional to operate effectively. The portable recording device captures patient video and audio, offering display and recording controls, as well as AI-enabled notifications for seizure activity4, crucial in critical or emergency scenarios5,6. ONE seamlessly streams data to the Zeto Cloud, enabling live remote interpretations by board-certified neurologists. In addition to its role as a point-of-care system, it serves as a comprehensive EEG platform, enabling various tasks such as workflow management, patient scheduling, and report generation.
Susan Herman, M.D., Professor and Vice Chair of Clinical Affairs, Department of Neurology at Barrow Neurological Institute said, “Zeto ONE is a breakthrough EEG system, revolutionizing many aspects of emergency EEG acquisition. We know that up to 40% of brain injured emergency department and intensive care patients may experience seizures, which are often subclinical and require EEG for diagnosis. ONE fills a gap for hospitals that lack EEG resources – provides streamlined point-of care application of full 10-20 electrodes, video and audio recording, AI triage tools, and efficient connectivity to the interpreting neurologist. This enhanced workflow ensures that EEGs have high technical quality and accurate interpretations in our most critically ill patients.”
Zeto’s Founder and CEO, Aswin Gunasekar stated, “Breakthrough changes arise from the cumulative effect of years of gradual improvements. ONE is a culmination of 8+ years of customer centric product development by our industrious team. As our first-generation Wrap (WR19) headset sees increasing adoption for short-term EEGs, ONE strengthens our portfolio by democratizing access to continuous EEG brain monitoring and diagnostics. We anticipate ONE to notably advance EEG monitoring in critical care, outpatient and home settings.”
Christina Patterson, MD, Associate Professor of Pediatrics and the Director of the Epilepsy Center at UPMC Children’s Hospital of Pittsburgh said, “Zeto ONE will be a profound help to our pediatric patients by increasing access to much needed diagnostic and therapeutic interventions, particularly in Emergency Departments and Intensive Care Units where rapid application and complete EEG can make all the difference in getting a critically ill child the care they need.”
“Many hospitals in the world have no ability to obtain EEGs.,” said Robert S. Fisher, M.D., Ph.D., Director of the Stanford Epilepsy Center and former President of the American Epilepsy Society. “Zeto ONE will make it possible for them to do so. For hospitals and offices with EEG capabilities, ONE will make obtaining the EEG more efficient for the medical personnel and more comfortable for the patients.”
Zeto ONE is now available for sale. For inquiries, please call: +1 (866) 527-5549, +1 (833) ZETO EEG or email: sales@zetoinc.com
References:
- Herman, S.T., et al. (2015). “J Clin Neurophysiol,” 32(2):87-95.
- Kolls, B.J., and Husain, A.M. (2007). “Epilepsia,” 48(5):959-65.
- Klem, G.H., Lüders, H.O., et al. (1999). “Guidelines of the International Federation of Clinical Physiology,” EEG Suppl. 52.
- Enabled by Encevis. Rommens, N., et al. (2018). “Improving staff response to seizures on the epilepsy monitoring unit with online EEG seizure detection algorithms,” Epilepsy & Behavior, July 2018.
- Hillman, J., et al. (2013). “National Library of Medicine,” 6(6).
- Madžar, D., et al. (2016). “J Neurol,” 263:485-491.
About Zeto, Inc.
About Zeto, Inc.
Zeto, Inc., an award-winning medical technology firm, is at the forefront of advancing EEG brain monitoring and diagnostics for healthcare. Offering wearable devices, Zeto makes brain monitoring accessible across various clinical settings including the ICU, ED, hospital, office, and home. Supported by a feature-rich cloud-based platform, Zeto provides nationwide monitoring and interpretation services rendered by neurologists, alongside AI-enabled notifications for conditions such as seizures and epilepsy. Zeto plans to expand its capabilities in the future to recognize and manage conditions such as depression and traumatic brain injury.
To learn more about Zeto’s products, please visit: https://zeto-inc.com or email us at info@zetoinc.com.
Source – PRNewswire