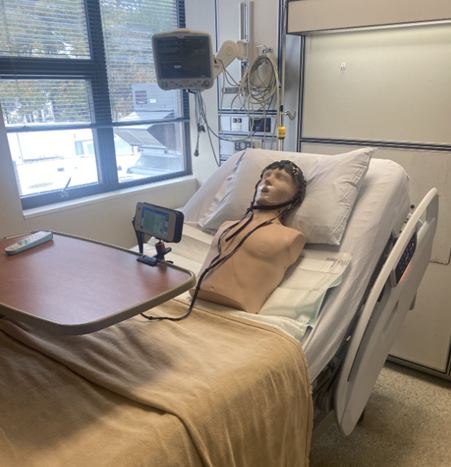
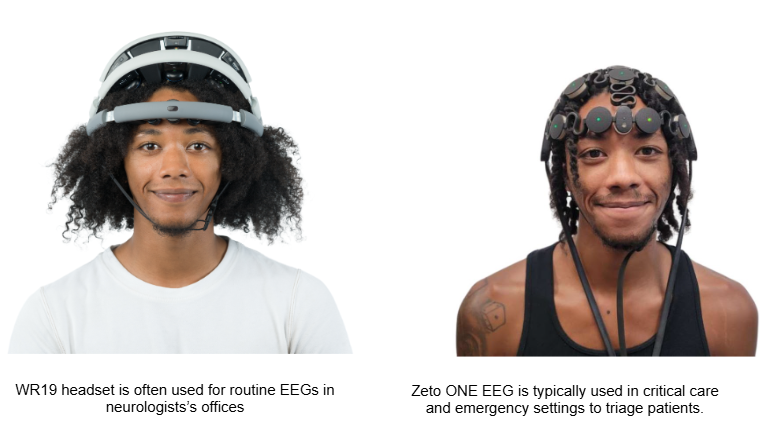
Zeto ONE makes it possible for nursing staff to initiate high-quality EEGs—no gel, no wires—when EEG technologists are unavailable.
In many hospitals, especially in emergency departments, intensive care units, and rural facilities, nurses are often the first clinicians to respond when a patient shows signs of a neurological emergency—such as nonconvulsive seizures, status epilepticus, or post–cardiac arrest encephalopathy. But traditional EEG systems are generally not deployed by nurses. They require EEG technicians – critical practitioners who unfortunately may not be always available in rural settings or off-hours.
Zeto ONE offer Rapid FULL Montage EEG for the ICU
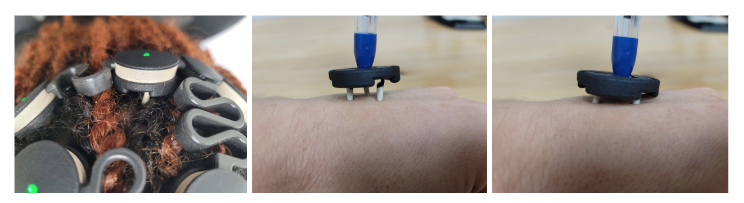
It is the first FDA-cleared, full-montage EEG system that can be applied by trained nursing staff when EEG techs are unavailable—without requiring gels, glues, or specialized tools. The system is intuitive and wireless, enabling clinicians to initiate EEGs within minutes, even in critical care environments.
EEG technologists remain the gold standard in the administration of EEG studies. Zeto ONE offers EEG techs, and when they’re not available, other front-line staff such as nurses, an invaluable and easy to use tool when time to treatment is critical, and expert personnel are not immediately on-site.
Why Fast EEG Access Matters
EEG plays a vital role in diagnosing seizures—especially nonconvulsive seizures and nonconvulsive status epilepticus, which can be difficult to identify through clinical observation alone. In neurocritical care and emergency medical settings, delayed EEG access can delay treatment, particularly for patients in altered mental states following epileptic seizures or cardiac arrest.
Traditional EEG systems require:
- Specialized EEG technologists for setup and monitoring
- 15–20 minutes or more for electrode placement
- Gels, wires, and post-procedure cleanup
In the absence of an EEG tech, clinicians must either wait until they are available, which could be days, or transfer the patient— a time-intensive and resource-draining process.
With Zeto ONE, trained nurses can initiate EEGs in under five minutes, helping reduce diagnostic delays and supporting earlier intervention.
Zeto ONE: A Nurse-Friendly EEG System, Not a Replacement for Technologists
Zeto ONE is user-friendly enough to be deployed by neuro-ICU nurses, emergency teams, or critical care staff with minimal training. When EEG techs are unavailable, it enables immediate EEG acquisition that can be reviewed by physicians or EEG personnel remotely.
Key features include:
- Full-montage high-quality EEG
- Application in under 5 minutes—no gels, wires, or prep
- Comfortable for supine patients in ICUs or emergency bays
- Portable, compact headset fits seamlessly into crowded units
- Quick to remove and reapply
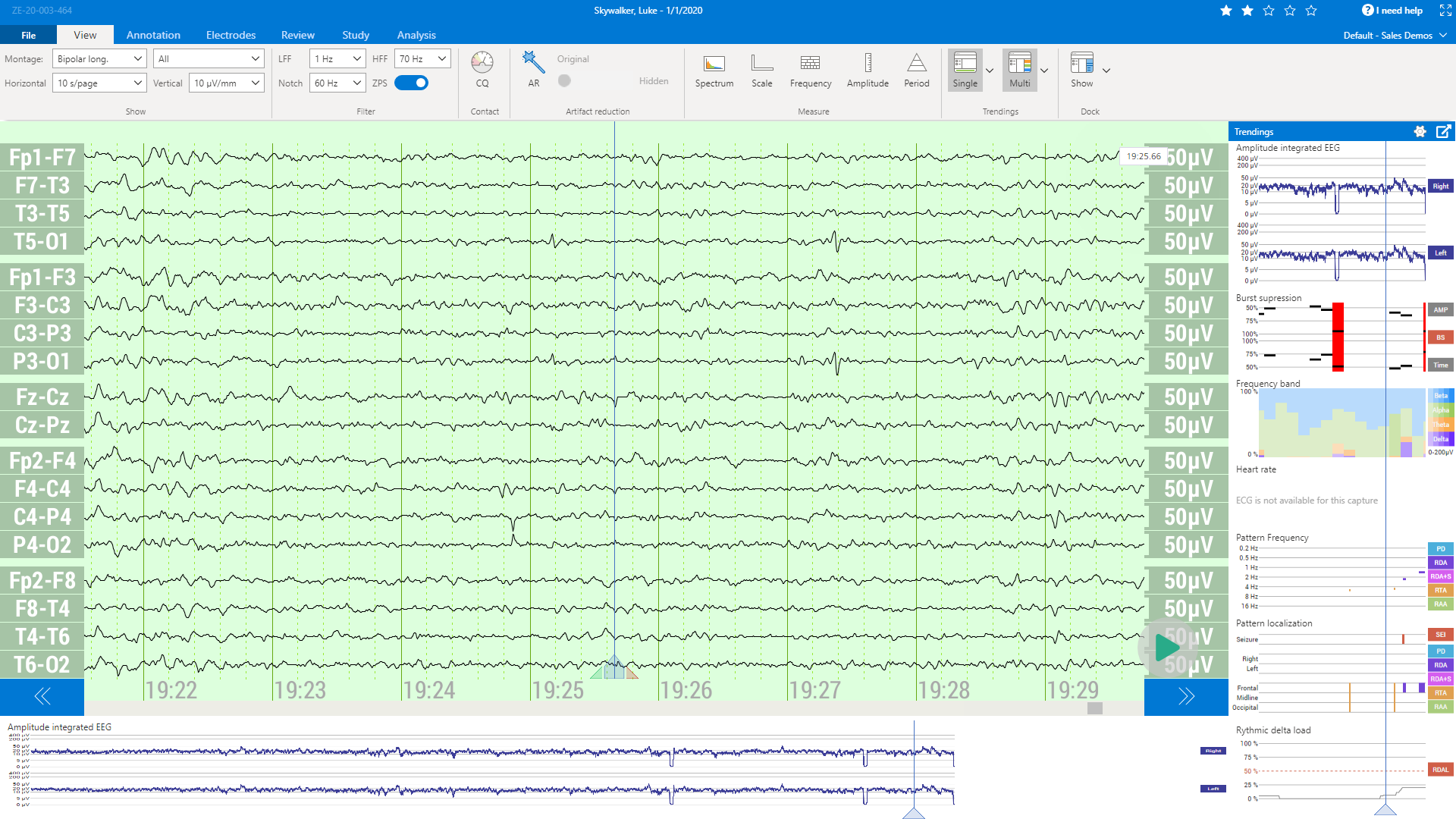
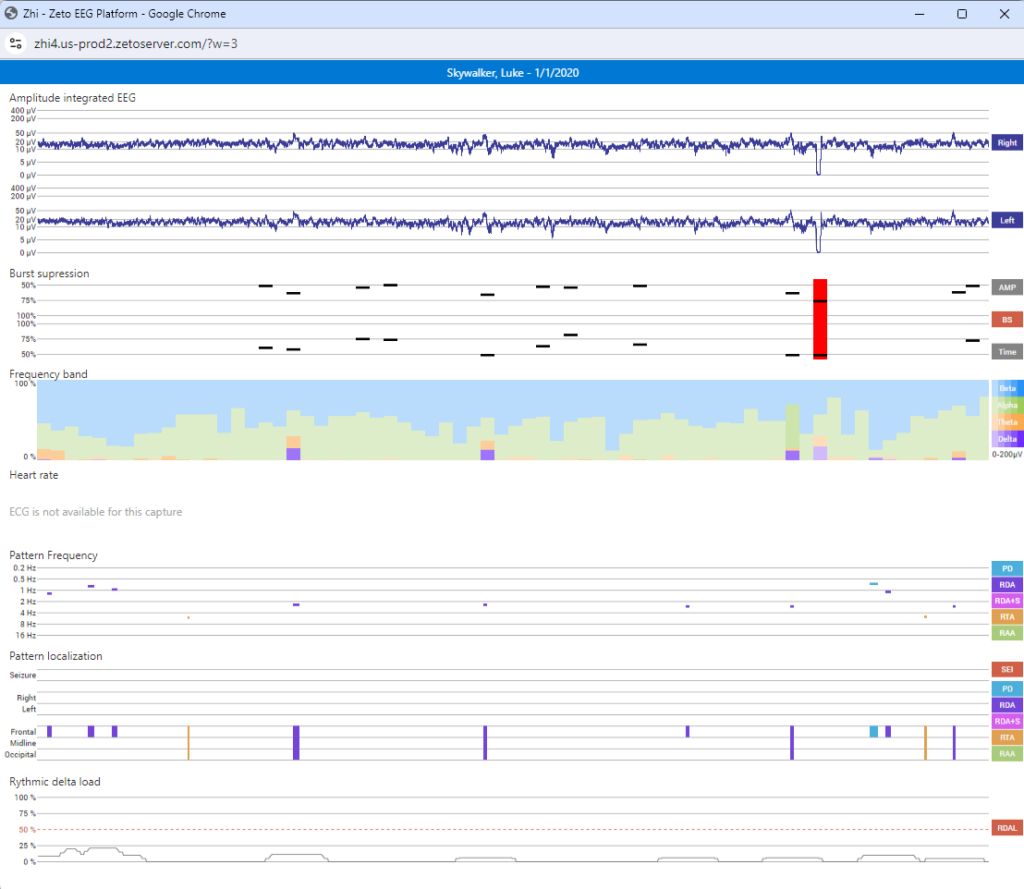
Once applied, Zeto ONE begins recording immediately, sending data to a secure cloud-based platform that enables remote access for neurologists and EEG staff for interpretation.
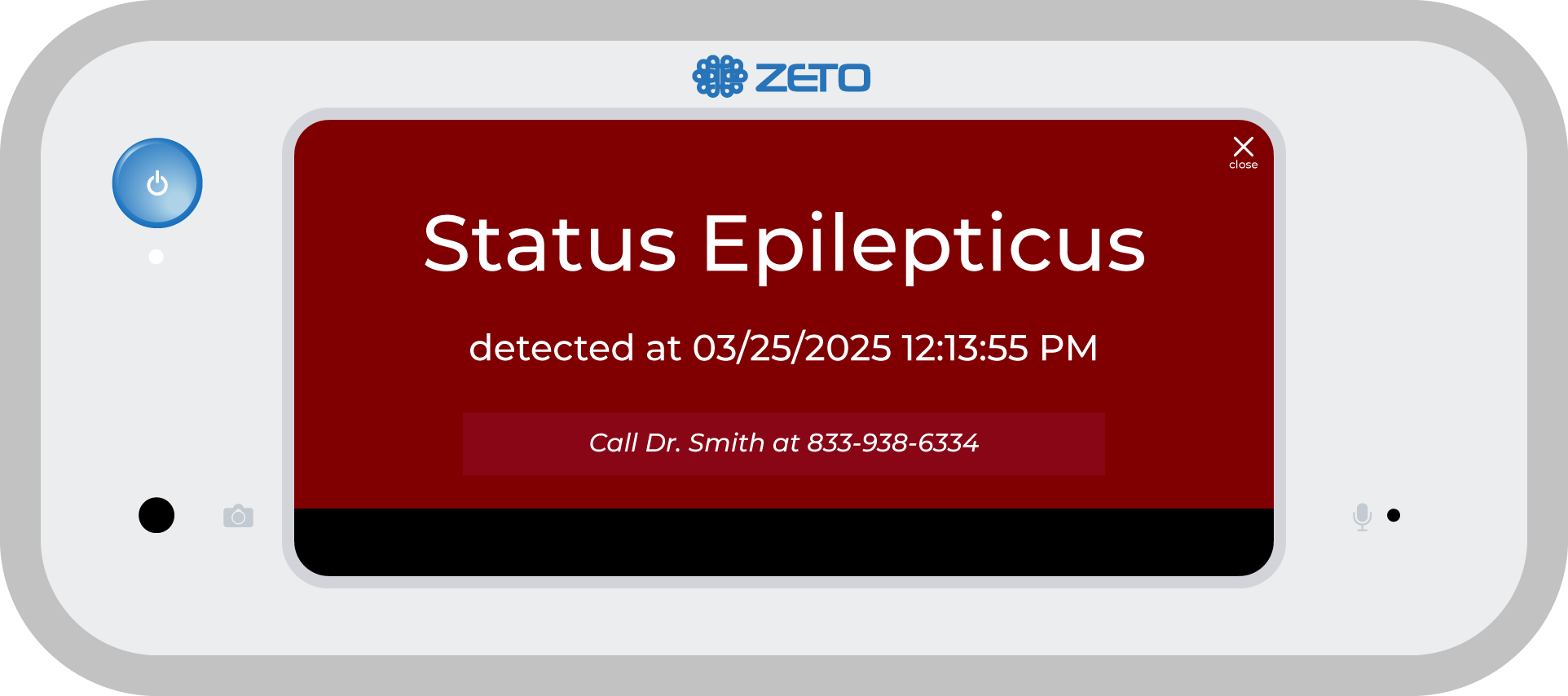
Built-In Seizure Detection with NeuroPulse AI™
Zeto ONE includes NeuroPulse AI™, an AI-powered seizure detection tool trained on more than 21,000 hours of EEG recordings across over 800 patients. It continuously monitors for abnormal brain activity and automatically alerts care teams.
If seizure activity is detected:
- Nurses receive a notification at the bedside
- Physicians and EEG techs can be notified remotely
This capability empowers nursing staff to identify and respond to neurological deterioration, even in the absence of on-site specialists.
Streamlining Workflow for Nurses in Critical Care
Zeto ONE is designed to work within the constraints of busy, high-acuity units:
- EEG studies are immediately available to remote neurologists
- NeuroPulse AI™ generates real-time summaries and insights
- No need to transport patients only to get EEG or coordinate external EEG services
It’s especially valuable during night shifts, weekends, or in smaller facilities without 24/7 neurology or EEG coverage.
Additionally, the system is:
- Quick to remove and reapply for imaging procedures
- Compact enough to store and charge within neurocritical care units
- Non-disruptive to existing care protocols
Easy to Clean: A 5-Minute Protocol
Zeto ONE is also easy to maintain, with cleaning protocols that meet infection control standards without consuming staff time.
Our happy customer at Huntsville Memorial Hospital (HMH) in Texas, shared with us that their staff follow a 5-minute cleaning process that has passed routine inspections by their infection control nurse.
The process:
- Step 1: Remove the headset—no gel, no residue, no skin irritation
- Step 2: Wipe down the device using hospital-approved SaniWipes
- Step 3: Use 70% isopropyl alcohol
“Cleaning takes about five minutes. We use hospital-approved wipes to reach all areas. Infection control inspected and approved the process.”
— Joe Schorre, Director of Cardiopulmonary and Emergency Management, HMH
Additional notes:
- Cleaning is performed by respiratory techs or nurses immediately after use
- Devices are stored in designated, upright positions for charging and longevity
The result is a workflow-friendly process that supports rapid turnover between patients.
Conclusion: A Critical Tool for Emergency Gaps
EEG techs are indispensable, and Zeto ONE is not a substitute for their expertise. But in moments when rapid neurological insight is needed—and a tech isn’t available—Zeto ONE gives nurses a fast, accessible solution.
By empowering nurses to apply EEGs in urgent moments, Zeto ONE helps prevent treatment delays, reduce unnecessary transfers, and improve outcomes in emergency and intensive care settings.
Want to see how Zeto ONE fits into your neurocritical care workflow?
Schedule a demo or explore our quick-start training resources.