The dry electrode EEG system is a new development in the field of diagnostic science, offering an alternative to the conventional wet electrode EEG system.
To replace the wet EEG setup in clinical settings, dry electrode headsets must convey high-quality signals and give accurate results in terms of latency and amplitude. The dry electrode systems must also be able to separate biological signals from background noise.
Before comparing these two approaches, it is important to understand how each one of them works.
A brief overview of the wet EEG device
The traditional EEG system consists of small metal discs (electrodes), covered with a silver/silver-chloride coating, which are placed on the scalp. Some recording systems use elastic head caps, which have electrodes built-in in preset positions, expediting the correct electrode placement according to the 10-20 international standard, assuming a proportional expansion and distribution of electrodes over different head sizes.
Other, more traditional approaches, place single leads on the scalp one at a time using glue, gauze, and tape. An electrode gel is applied to the skin under the electrode to improve the skin-electrode conductivity and to reduce impedance. It also decreases the artifacts produced by the movements of electrode cables.
Once the electrodes are positioned, it often requires scraping the surface of the skin using various tools to remove the upper layer of skin to improve the conductivity between the skin and the gel.
Then the electrode is ready for recording the brain’s electrical activity and analyzing the data for diagnostic purposes.
A brief overview of the dry EEG device
In contrast to traditional electrodes, dry EEG systems make contact directly with the scalp and do not require conductive gel to be applied between the skin and electrode. That is made possible because of additional system components that increase the EEG signal strength right at the scalp.
Since they do not require any skin preparation, dry electrodes make the EEG headset suitable for rapid EEG tests, eventually, beyond healthcare facilities. The dry electrodes are easy to place without the help of any additional instruments like syringes or gel cans.
Moreover, after use, there is no need to clean the head as dry electrodes leave no residue on the skin or on the hair. Because dry electrodes are often made of plastic, they are affordable and can be made disposable, hence their use is a lot more hygienic and safer to be transferred between patients than traditional multiple-use electrodes.
Comparison of the dry and wet EEG system
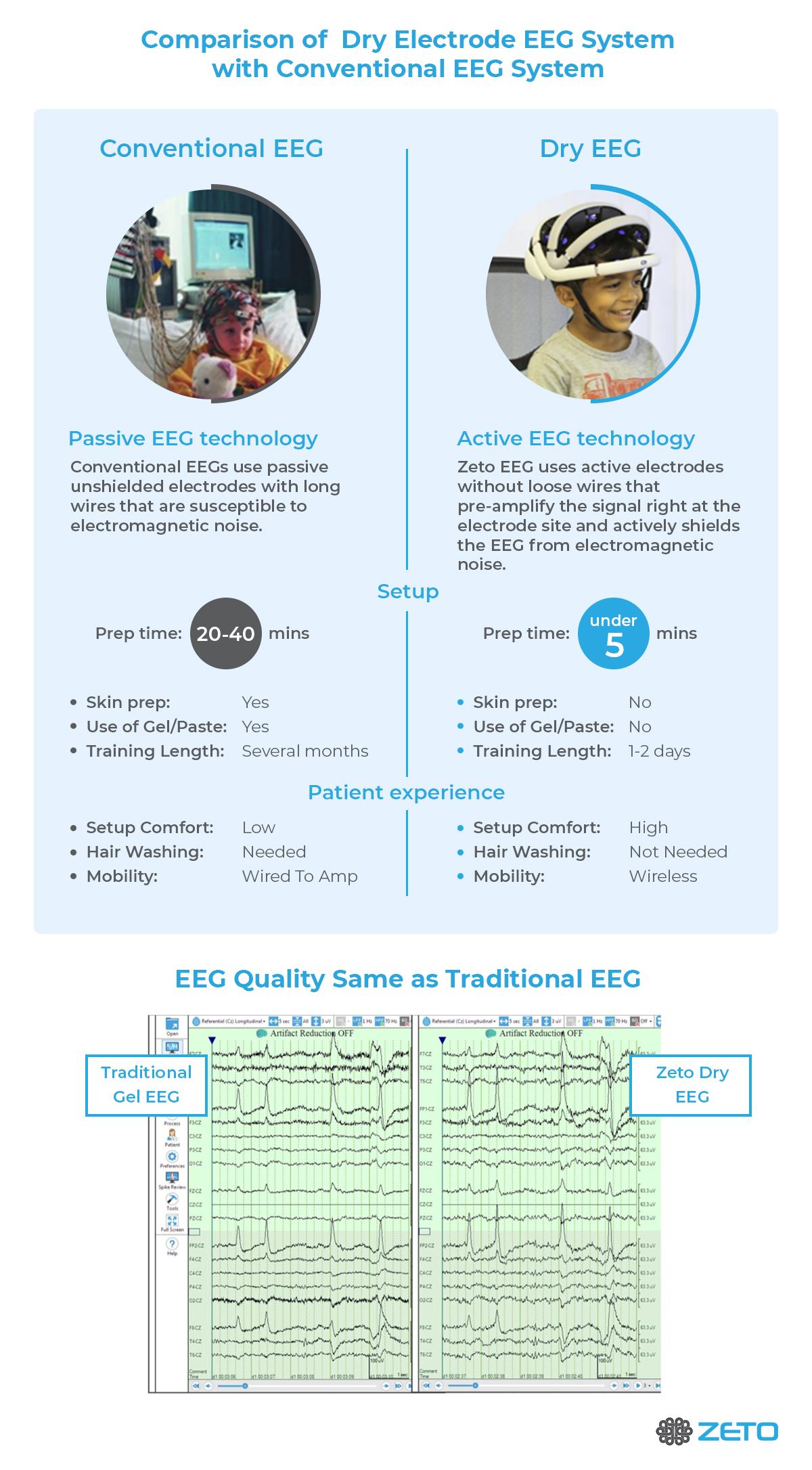
The main purpose of introducing dry electrodes to be used in EEG systems was to improve the comfort of patients and experimental subjects while reducing the time of preparation. The dry electrodes are cleaner, more comfortable, quicker to set up and quicker to remove. In short, they are more practical.
In addition to convenience and comfort, there are additional requirements a good clinical electrode has to meet.
An ideal dry EEG headset should stay on the patient’s head for hours to days or even weeks or more to ensure uninterrupted monitoring of the brain’s electrical activity.
To achieve this in clinical practice, EEG technicians glue the electrodes one by one to the skin with a collodion adhesive, apply the gel and cover the electrodes with a gauze bandage. The drawback of this method is that the gel dries quickly and needs to be replaced every few hours, which requires a trained EEG technologist to do as the head bandage needs to be replaced too.
Therefore, while this type of traditional wet electrode system is acceptable in the clinical settings where EEG technologists are available around the clock, this dependency on skilled labor makes EEG underutilized in many clinical areas, such as ICU, ED, NICU, and stroke centers, to name a few.
In contrast, dry electrode systems do not require an EEG technologist’s assistance to replace the electrodes. Introducing dry electrodes to clinical EEG monitoring, including long-term EEG, would not only free up the time of EEG technologists for EEG monitoring and allow them to complete more EEG studies but would also expand the use of EEG in clinical areas and clinics lacking EEG specialists on site.
Acceptance of the dry electrode systems in the clinical EEG market
Although dry electrode EEG headset systems have multiple advantages over gel-based electrodes, there is a barrier to widespread acceptance.
According to conventional wisdom, the lower the impedance of electrodes the better the quality of the recording is. However, recent technological advances have brought about a new generation of amplifiers capable of amplifying the signal orders of magnitude better than conventional systems and overcoming the impedance-gap of dry electrodes.
In addition, the introduction of active electrode technology, i.e. giving the EEG signal more strength by pre-amplifying the signal close to the electrode, ensures that the biological signal will not be affected by external electromagnetic noise before reaching the second amplifier stage. Conventional EEGs use passive electrodes, which makes the few micro-volt magnitude signals traveling in long cables from the electrode to the amplifier susceptible to electromagnetic noise especially upon movement of the cables.
Moreover, the active electrodes technology applies a driven current to each electrode that is being modulated by the brain’s electrical activity. The modulated signal will be detected by the electrodes and transferred to the amplifiers where the driven current will be subtracted from the signal to recover the brain’s original signal.
In addition to active electrode technology, dry electrode systems need good noise shielding and noise cancellation. As the biosignal travels through ‘unprepared’, high impedance skin layer, it becomes vulnerable to external noise such as 60Hz lines noise or other electrical interference in the room. Hence excellent shielding mechanisms are needed to protect the electrodes.
Moreover, the system needs to incorporate dynamic common mode noise rejection circuitry to improve CMRR (Common Mode Rejection Ratio) above 130dB which allows signal quality to be on par with traditional wet EEG systems.
The Benefits of Dry EEG Headsets
The combination of these technologies makes dry electrodes not only on a par with conventional electrode recording quality but able to exceed that.
As of today, many well-controlled and peer-reviewed studies have proven that dry electrode EEG headset systems are non-inferior to the conventional EEG and they are rapidly improving (Guger, Krausz, Allison, & Edlinger, 2012) (Di Flumeri et al., 2019; Fiedler et al., 2014; Hinrichs et al., 2020; Kam et al., 2019; Leach, Chung, Tüshaus, Huber, & Karlen, 2020; Li, Wu, Xia, He, & Jin, 2020; Mathewson, Harrison, & Kizuk, 2017; Schwarz, Escolano, Montesano, & Müller-Putz, 2020; Shad, Molinas, & Ytterdal, 2020; Zander et al., 2011).
The complicated nature of wet EEGs means they’re limited in the number of people they can reach. Extensive prep is needed, and this requires EEG technologists on hand at every step of the way. This limitation means EEGs can’t be rolled out in many settings where they can be most useful (ICU, ED, NICU, stroke centers, etc).
Dry EEG headsets solve this problem by making the setup simple. The average prep time is just five minutes, and the headset is comfortable for the patient, with gentle support pads making the process much more pleasant.
Of course, this wouldn’t be useful unless the results were accurate, and this is where the hard work has gone on behind the scenes. With technological improvements, studies are showing that results from EEG headsets are on par with conventional EEGs.
By combining accurate results with much-improved convenience, dry EEG headsets represent a great step forward in the way we can study the brain.
Zeto Wireless EEG Headset
The Zeto wireless EEG headset is the first FDA-approved true dry electrode EEG system.
Traditional EEG systems have clear drawbacks, and many hospitals and clinics have been eagerly awaiting a better EEG testing option. That options arrived in 2020, as Zeto’s EEG headset brought new levels of convenience combined with exceptionally accurate results.
The headset offers:
- Wireless, battery-powered
- No skin-prep, no cleanup
- Comfortable, no residue, soft tip electrodes
- Adjustable headset for child to adult sizes
- Precision placement as per 10-20 system
- Easy to learn for anyone familiar with EEG
Live remote viewing of video EEG can be accessed through the cloud allowing for seamless data management, and a mobile EEG system.
Don’t be limited by a shortage of EEG technologists, discover the Zeto wireless EEG headset.
Infographic – Comparison of Dry Electrode EEG System with Conventional System
References
Di Flumeri, G., Aricò, P., Borghini, G., Sciaraffa, N., Di Florio, A., & Babiloni, F. (2019). The Dry Revolution: Evaluation of Three Different EEG Dry Electrode Types in Terms of Signal Spectral Features, Mental States Classification and Usability. Sensors (Basel, Switzerland), 19(6), 1365. https://doi.org/10.3390/s19061365
Fiedler, P., Haueisen, J., Jannek, D., Griebel, S., Zentner, L., Vaz, F., & Fonseca, C. (2014). Comparison of three types of dry electrodes for electroencephalography. In Acta IMEKO. https://doi.org/10.21014/acta_imeko.v3i3.94
Guger, C., Krausz, G., Allison, B., & Edlinger, G. (2012). Comparison of Dry and Gel Based Electrodes for P300 Brain–Computer Interfaces. Frontiers in Neuroscience, 6, 60. https://doi.org/10.3389/fnins.2012.00060
Hinrichs, H., Scholz, M., Baum, A. K., Kam, J. W. Y., Knight, R. T., & Heinze, H. J. (2020). Comparison between a wireless dry electrode EEG system with a conventional wired wet electrode EEG system for clinical applications. Scientific Reports. https://doi.org/10.1038/s41598-020-62154-0
Kam, J. W. Y., Griffin, S., Shen, A., Patel, S., Hinrichs, H., Heinze, H.-J., … Knight, R. T. (2019). Systematic comparison between a wireless EEG system with dry electrodes and a wired EEG system with wet electrodes. NeuroImage, 184, 119–129. https://doi.org/10.1016/j.neuroimage.2018.09.012
Leach, S., Chung, K., Tüshaus, L., Huber, R., & Karlen, W. (2020). A Protocol for Comparing Dry and Wet EEG Electrodes During Sleep. Frontiers in Neuroscience, 14, 586. https://doi.org/10.3389/fnins.2020.00586
Li, G.-L., Wu, J.-T., Xia, Y.-H., He, Q.-G., & Jin, H.-G. (2020). Review of semi-dry electrodes for EEG recording. Journal of Neural Engineering, 17(5), 51004. https://doi.org/10.1088/1741-2552/abbd50
Mathewson, K. E., Harrison, T. J. L., & Kizuk, S. A. D. (2017). High and dry? Comparing active dry EEG electrodes to active and passive wet electrodes. Psychophysiology, 54(1), 74–82. https://doi.org/10.1111/psyp.12536
Schwarz, A., Escolano, C., Montesano, L., & Müller-Putz, G. R. (2020). Analyzing and Decoding Natural Reach-and-Grasp Actions Using Gel, Water and Dry EEG Systems. Frontiers in Neuroscience, 14, 849. https://doi.org/10.3389/fnins.2020.00849
Shad, E. H. T., Molinas, M., & Ytterdal, T. (2020). Impedance and Noise of Passive and Active Dry EEG Electrodes: A Review. IEEE Sensors Journal, 20(24), 14565–14577. https://doi.org/10.1109/JSEN.2020.3012394
Zander, T., Lehne, M., Ihme, K., Jatzev, S., Correia, J., Kothe, C., … Nijboer, F. (2011). A Dry EEG-System for Scientific Research and Brain–Computer Interfaces. Frontiers in Neuroscience, 5, 53. https://doi.org/10.3389/fnins.2011.00053