Introduction
EEGs are an invaluable tool for monitoring real-time brain function at the bedside in the ICU.
Nonconvulsive seizures and nonconvulsive status epilepticus in the ICU are very shockingly common. Now that continuous EEG monitoring (cEEG) has entered clinical practice, we know the incidence of nonconvulsive seizures is between 8% and 37% of ICU patients.1 Up to 22% of patients in the medical ICU without brain injury have periodic discharges or seizures.2 Up to 16% of patients in the surgical ICU have seizures.3
Nonconvulsive seizures and nonconvulsive status epilepticus are extremely hard to detect at the ICU bedside—physicians missed 88% of these cases in one retrospective study.4 Sadly, delays in diagnosing and treating nonconvulsive status epilepticus treatment are associated with poor patient outcomes.5,6 Because of this dire need, professional societies and experts are calling on ICU staff to routinely order EEG monitoring in critical care units.7-9

Why order EEG in the ICU?
Seizures and/or status epilepticus causes neuronal damage10 and in some cases, hippocampal atrophy.11 These treatable conditions lead to poor outcomes in both children and adults. Prolonged seizures are associated with chronic cognitive problems and neurological sequelae . In short, undiagnosed and untreated seizures are dangerous for patients.
Making matters worse, seizures are often missed in the ICU setting when the diagnosis is based on clinical signs alone.4 Indeed, as Dr. Lawrence J. Hirsch of the Comprehensive Epilepsy Center of Columbia University in New York put it, “it is fair to say that anyone who works with critically ill neurologic patients and does not see nonconvulsive seizures and nonconvulsive status epilepticus on a regular basis is missing the diagnosis.”12
Given the complex nature of patients’ deficits in the ICU, it is unreasonable to rely on physical/neurological examination alone to detect nonconvulsive seizures.
EEG monitoring does appear to be better able to detect both subclinical seizures and subclinical status epilepticus compared to routine EEG according to a systematic review and meta-analysis study of over 20,000 critically ill adult patients.13
However, this might not translate into long-term clinical benefit, as suggested by a recent multicenter randomized clinical trial in Switzerland called the CERTA study, which evaluated 364 patients using continuous EEG or two routine 20-minute EEGs. The researchers did not find that mortality significantly differed between the two groups at 6 months.
Nevertheless, Neurocritical Care Society guidelines recommend the institution of continuous EEG within an hour of suspecting status epilepticus in all patients.14 Availability of EEG technologists, who can set up a routine and continuous EEGs, play a vital role in enabling ICU EEG monitoring, yet only 26% of institutions have technologists accessible 24/7 in-house.15
According to a study of 625 critically ill patients, preliminary findings from the first minutes of EEG recording have a high predictive value in detecting patients at greater risk for seizures and who would benefit from long-term monitoring.16 The absence of epileptiform discharges after two hours of EEG recording reduced the probability of seizure occurrence to less than 5%, and less than 10% after only 15 minutes.
When to order EEG in the ICU
EEG should be ordered without delay for any ICU patient with suspected nonconvulsive seizures. As mentioned, however, clinical suspicion is not terribly reliable4, thus the bar for ordering cEEG in ICU patients should be very low.
Continuous EEG should be ordered in ICU patients with7,12
- Fluctuating mental status
- Head trauma
- History of convulsive seizures (especially convulsive status epilepticus; about one in two patients with coma and previous convulsive status epilepticus have nonconvulsive seizures.1)
- Ischemic stroke
- Intraparenchymal hemorrhage
- Aneurysmal subarachnoid hemorrhage
- CNS infection
- Brain tumor
- Sepsis
- Recent history of ECMO
- Hypoxic brain injury of any cause
Continuous EEG monitoring can help critical care physicians properly characterizing “spells” in the ICU “sudden posturing, rigidity, tremors, chewing, agitation, or sudden changes in pulse or blood pressure without an obvious explanation.”12 cEEG can also provide useful information about the level of sedation and can detect clinically silent, but significant neurologic events.12
How to get EEG in the ICU: Rapid EEG Solution
Rapid access to clinical EEGs in ICUs has a significant impact on diagnosis and outcomes in patients with seizures and acute neurological disorders. Despite the obvious need, it is still difficult for most critical care staff to get a rapid EEG in the ICU. The biggest hurdles to EEG in the ICU are a lack of dedicated EEG equipment and full-time staff that can run and read EEG and cEEG studies.
What is Rapid EEG?
- EEG performed acutely for new onset of patient events and/or seizures
- Designed to be started within a critical time window with the goal of triaging/treating sooner to prevent brain damage
- Can be placed quickly by bedside care providers
- May be in “screening-quality” category, or may be equivalent to standard EEG quality
How Zeto Can Help
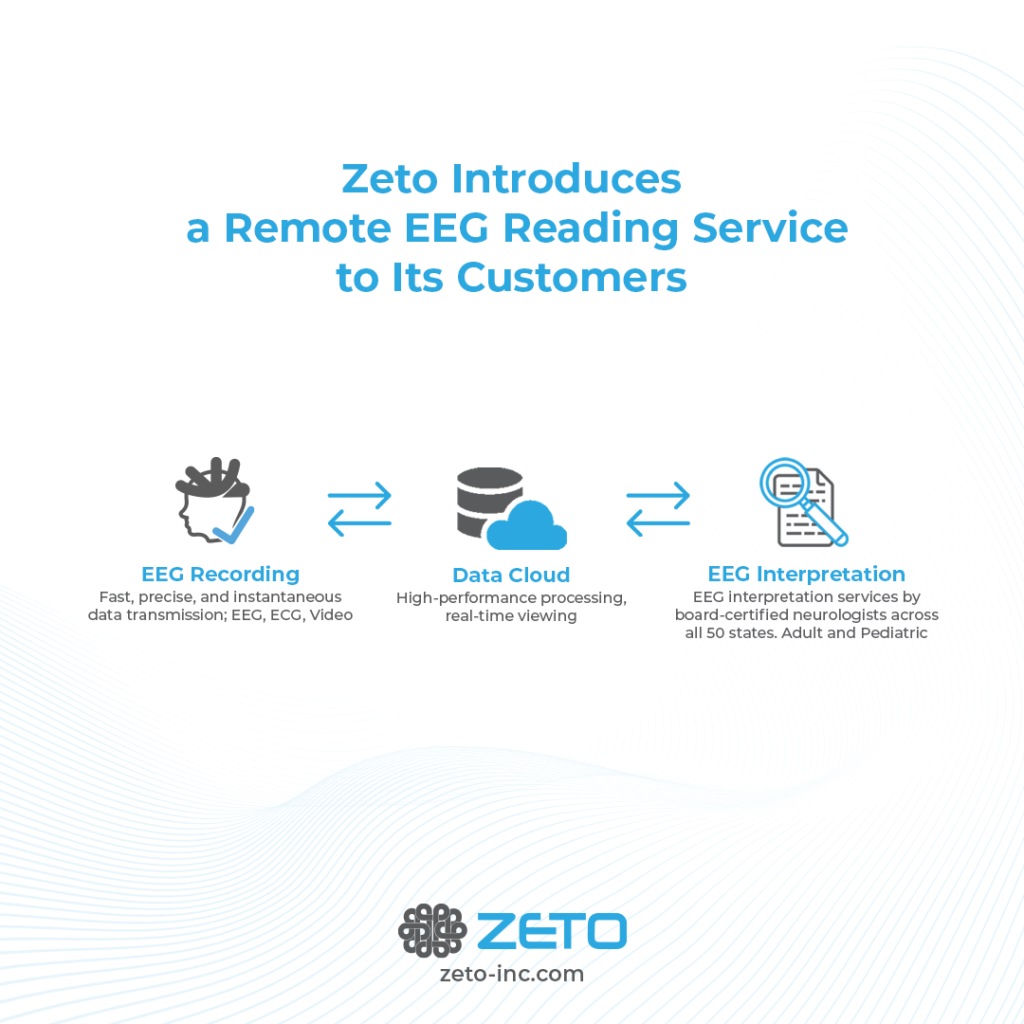
Zeto offers a rapid full montage EEG solution that can be easily deployed in the ICU without a dedicated technologist. Zeto might be used for cEEG for up to 4 hours and for routine EEG. Zeto EEG can provide accurate, high-quality, 19-channel medical-grade EEGs in a matter of minutes (average setup time is about 5 minutes) without skin prep or cleanup.
Virtually anyone who works in the ICU can place the Zeto device with minimal training, it’s possible to use cross-trained personnel. The Zeto team trains onsite and offers remote support.
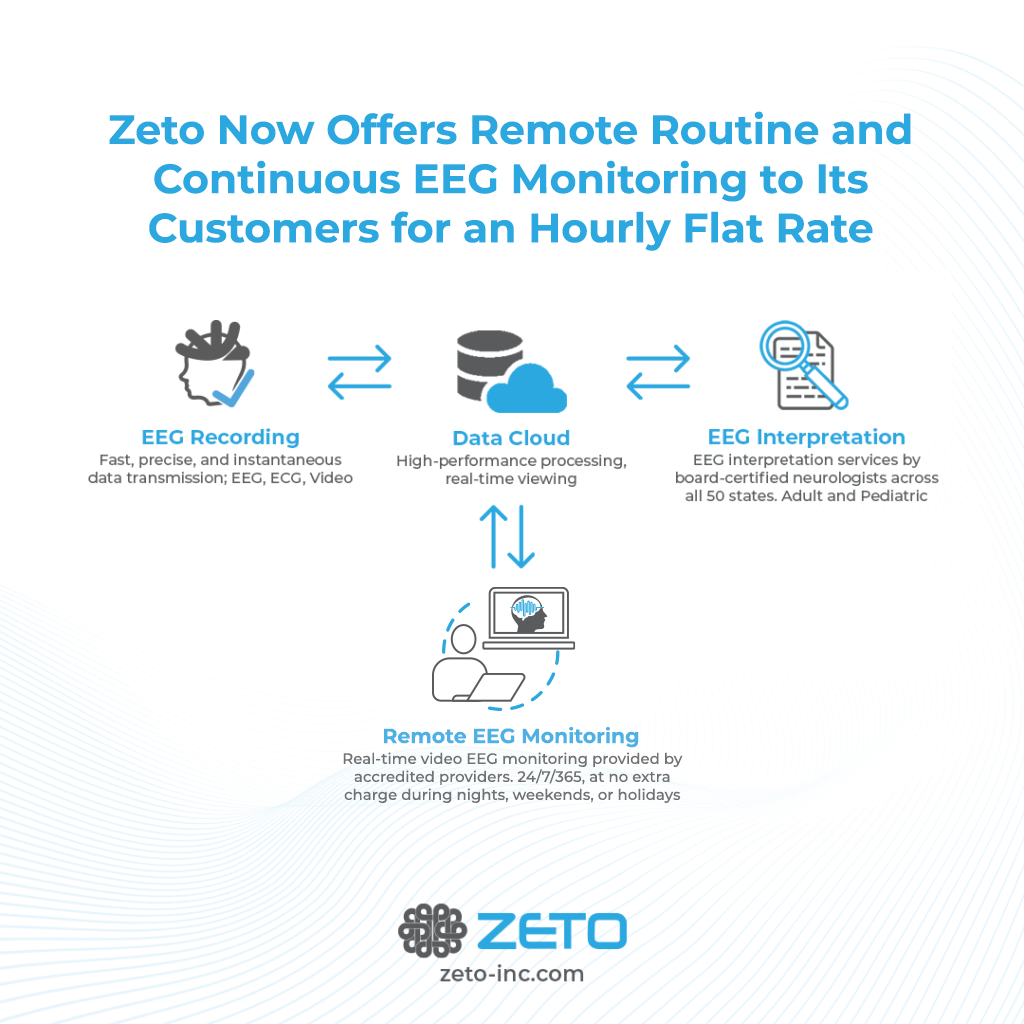
Once the wireless EEG system is placed on the patient’s head, the resulting EEG is available in real time for live monitoring. ICU staff has the additional paid-on option of real-time remote patient monitoring by registered EEG techs and short-notice remote reads by certified neurologists.
Most importantly, Zeto integrates FDA cleared Seizure Detection and continuous Seizure Load monitoring tools from encevis into its User Interface for automatic detection/notification of such critical events, providing more integrated functionality vs. competitors.
With Zeto, it is now possible to obtain medical-grade EEGs in the ICU setting without an on-site EEG staff. Within minutes, our integrated EEG solution notifies staff of continuous seizures enabling physicians to intervene in a timely manner and save lives in critical care settings.
References
1. Kennedy JD, Gerard EE. Continuous EEG monitoring in the intensive care unit. Curr Neurol Neurosci Rep. 2012;12(4):419-428. 10.1007/s11910-012-0289-0
2. Oddo M, Carrera E, Claassen J, Mayer SA, Hirsch LJ. Continuous electroencephalography in the medical intensive care unit. Crit Care Med. 2009;37(6):2051-2056. 10.1097/CCM.0b013e3181a00604
3. Kurtz P, Gaspard N, Wahl AS, et al. Continuous electroencephalography in a surgical intensive care unit. Intensive Care Med. 2014;40(2):228-234. 10.1007/s00134-013-3149-8
4. Drislane FW, Lopez MR, Blum AS, Schomer DL. Detection and treatment of refractory status epilepticus in the intensive care unit. J Clin Neurophysiol. 2008;25(4):181-186. 10.1097/WNP.0b013e31817be70e
5. Pang T, Hirsch LJ. Treatment of Convulsive and Nonconvulsive Status Epilepticus. Curr Treat Options Neurol. 2005;7(4):247-259. 10.1007/s11940-005-0035-x
6. Trevathan E. Ellen R. Grass Lecture: Rapid EEG analysis for intensive care decisions in status epilepticus. Am J Electroneurodiagnostic Technol. 2006;46(1):4-17.
7. Herman ST, Abend NS, Bleck TP, et al. Consensus statement on continuous EEG in critically ill adults and children, part I: indications. J Clin Neurophysiol. 2015;32(2):87-95. 10.1097/WNP.0000000000000166
8. Herman ST, Abend NS, Bleck TP, et al. Consensus statement on continuous EEG in critically ill adults and children, part II: personnel, technical specifications, and clinical practice. J Clin Neurophysiol. 2015;32(2):96-108. 10.1097/WNP.0000000000000165
9. Rossetti AO, Hirsch LJ, Drislane FW. Nonconvulsive seizures and nonconvulsive status epilepticus in the neuro ICU should or should not be treated aggressively: A debate. Clin Neurophysiol Pract. 2019;4:170-177. 10.1016/j.cnp.2019.07.001
10. Palmio J, Keränen T, Alapirtti T, et al. Elevated serum neuron-specific enolase in patients with temporal lobe epilepsy: A video–EEG study. Epilepsy research. 2008;81(2-3):155-160.
11. Vespa PM, McArthur DL, Xu Y, et al. Nonconvulsive seizures after traumatic brain injury are associated with hippocampal atrophy. Neurology. 2010;75(9):792-798. 10.1212/WNL.0b013e3181f07334
12. Hirsch LJ. Continuous EEG monitoring in the intensive care unit: an overview. J Clin Neurophysiol. 2004;21(5):332-340.
13. Sharma, S., Nunes, M., & Alkhachroum, A. (2022). Adult Critical Care Electroencephalography Monitoring for Seizures: A Narrative Review. Frontiers in Neurology, 13.
14. Brophy, G. M., Bell, R., Claassen, J., Alldredge, B., Bleck, T. P., Glauser, T., … & Vespa, P. M. (2012). Guidelines for the evaluation and management of status epilepticus. Neurocritical care, 17(1), 3-23.
15. Gavvala, J., Abend, N., LaRoche, S., Hahn, C., Herman, S. T., Claassen, J., … & Critical Care EEG Monitoring Research Consortium (CCEMRC). (2014). Continuous EEG monitoring: a survey of neurophysiologists and neurointensivists. Epilepsia, 55(11), 1864-1871.
16. Rubinos, C., Alkhachroum, A., Der-Nigoghossian, C., & Claassen, J. (2020, December). Electroencephalogram monitoring in critical care. In Seminars in neurology (Vol. 40, No. 06, pp. 675-680). Thieme Medical Publishers, Inc.