Small Hospitals, Big Shifts:
RTs and the EEG Frontier
How one respiratory therapist became his hospital’s EEG expert – and what it means for rural healthcare
Daniel Rhoades never expected to become an EEG technologist. For 28 years, he’s worked as a respiratory therapist at Western Reserve Hospital in Ohio, and for the past several years, he’s coordinated the hospital’s sleep lab. But when their registered EEG technologist left for medical school and didn’t return, Daniel found himself volunteering for an entirely new role.
“I was the lucky one to get trained on it,” Daniel says with characteristic modesty. “Now I’ve been doing it for a little over a year. I think I’ve got about 120 EEGs done so far with Zeto EEG headset, and I’m the only one that does them at the hospital.”
His story illustrates a growing trend in rural healthcare: when specialized technologists aren’t available, hospitals are turning to other skilled clinicians – and new technology – to fill critical gaps in patient care.
The Rural Hospital Reality
Western Reserve Hospital is a 100-bed community facility in Northeast Ohio facing the same challenge as many small hospitals nationwide. They once employed a dedicated EEG technologist who provided reliable service. But when she left for medical school, the hospital faced a decision that many rural facilities know well: hire a replacement for what might be sporadic EEG volume, or find another approach.
They chose innovation over tradition.
Daniel’s director, Matthew Smith, Senior Director of Ancillary Services, looked into Zeto’s wireless EEG system. After a demonstration, Daniel – with his extensive respiratory therapy and sleep lab background – stepped forward to learn the technology.
“For a hospital our size, it doesn’t make sense to hire another full-time EEG tech,” Daniel explains. “There may not be enough EEGs to keep someone busy all the time.”
Two Departments, Two Different Worlds
Over the past year, Daniel has performed approximately 120 inpatient EEG studies, averaging about five per week. The majority are ordered by the ICU (around 70%), with the emergency department accounting for about 10% and other inpatient units roughly 20%.
But the patients in these settings couldn’t be more different.
“All of the patients that I’ve done in the emergency room have been awake and somewhat alert,” Daniel notes. “Whereas most of the patients in ICU are unconscious and intubated, unable to communicate.”
In the ER, he typically sees elderly patients who fell at home – they got dizzy, fell down, and woke up on the floor without remembering what happened. These patients are conscious and can follow commands to perform EEGs.
The ICU tells a different story entirely. “ICU is more strokes, somebody overdosed, they’ve been without oxygen for a period of time or not breathing,” Daniel explains. “These patients are often unconscious, intubated, and surrounded by life-support equipment.”
His respiratory therapy background proves invaluable in these complex ICU environments. “I’m comfortable around ventilators, just working in respiratory,” he says. “I can make adjustments to the bed, keep an eye on the ET tube.”
The Mobile EEG Setup
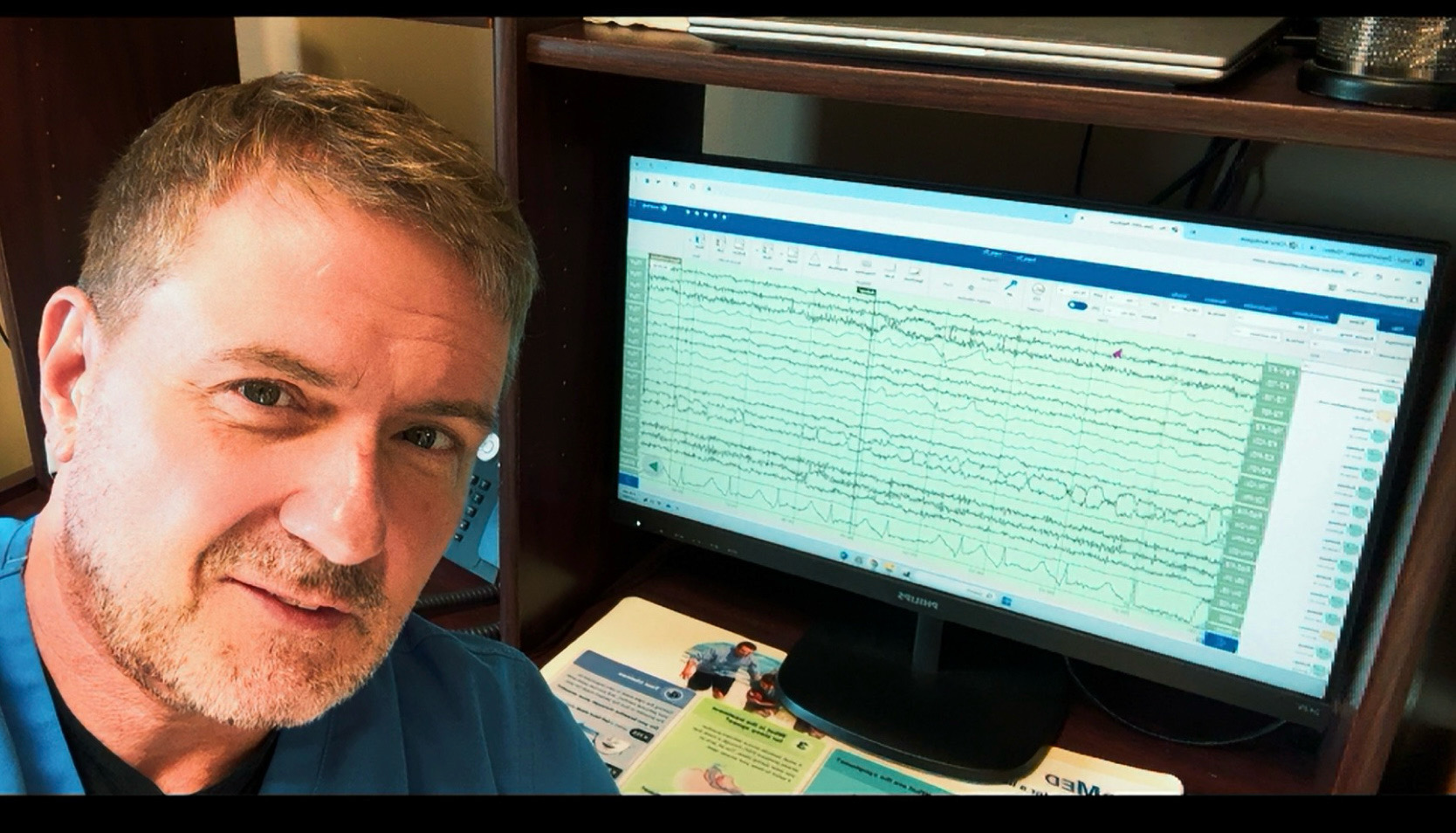
Daniel has organized everything he needs on a rolling cart: a dedicated laptop, Zeto headset and electrodes. When a physician calls for an EEG, he wheels his setup directly to the bedside – whether that’s the ICU, emergency room, or any other department.
The transformation from traditional EEG is dramatic. Where measuring heads, placing individual electrodes with paste, and connecting wires used to take up to an hour, Daniel can now complete setup in 10-15 minutes.
“I can input the patient data, get the helmet set up, and start a study within 15 minutes,” he says. Each study runs 30-40 minutes (always with video), during which Daniel adds frequent annotations to flag patient movements or anything unusual.
“I make lots of notes because I want to make sure that the physicians who aren’t there with me in the room understand what’s going on,” he explains. “I might see a twitch or somebody kicking their leg or moving. It’s really easy – I just right-click and a window pops up where I can add an annotation with a timestamp.”


When Wi-Fi Fails, Technology Prevails
The emergency room sits on the hospital’s bottom floor, where Wi-Fi signals sometimes weaken. But even when connectivity drops completely, Zeto keeps working.
“The headset connects to the laptop via WiFi, so even if the connection cuts out, it continues recording,” Daniel explains. “The study is stored temporarily and uploads automatically once WiFi is re-established. The physicians just have to wait a bit longer to see it, but we don’t lose any data.”
Quality Control and Patient Care
Perhaps most importantly, Daniel consistently delivers clinical-quality results. Zeto’s software includes a signal quality rating system, and Daniel tracks his performance carefully.
“I’ve averaged a four out of five stars over the past year with 120 studies under my belt,” he notes. “It’s pretty much the same quality no matter where I’m at – I could get about the same quality whether it’s ICU or ER.”
The neurologists who read his studies haven’t complained about quality either. “I haven’t had any complaints with the quality of the EEG,” Daniel says. “
Patient Experience Matters
When patients are alert enough to comment, their reactions are consistently positive – especially those who’ve had traditional EEGs before.
“Usually, the patients that have had previous old school EEGs are very pleased with not having to use collodion and having the glue in their hair,” Daniel observes. “They’re amazed by it – “Oh wow, there’s no glue involved, and they don’t have wires hanging all over the place.” It’s more of a positive experience.”
Even patients with challenging hair types haven’t posed significant problems. “I’ve had some patients with braids, but Zeto’s the electrodes have multiple contact points, so you can work a braid right through the contact points and still get a good connection,” he explains. “I’ve had some hair that was very thick, but I just parted the hair in the areas I needed to get contact.”
For patients, there’s also a comfort difference. “I’ve had patients complain about having little sores on their head where they were scrubbed with traditional EEGs,” Daniel notes. “This is nothing like that.”
The Productivity Revolution
The efficiency gains have been transformative for Daniel’s workflow. Where he estimates he could do maybe two traditional EEGs per day maximum – severely limiting his other responsibilities – he’s now completed up to five Zeto EEGs in a single day.
“If I had to hardwire those EEGs, that alone would limit me doing my other work,” he explains. “I would be lucky to be able to do a maximum of two maybe a day, whereas now I’ve done four or five. It definitely is helpful.”
This matters because Daniel isn’t just doing EEGs. He’s still coordinating the sleep center, scoring studies from the previous night, and setting up charts for upcoming nights.
The Bigger Picture
Daniel’s story represents more than one hospital’s creative solution to a staffing challenge. It illustrates how rural healthcare is evolving, with skilled clinicians taking on expanded roles enabled by user-friendly technology.
“I think anybody could learn how to use this equipment properly,” Daniel reflects. “I’m more of a hands-on person – I need to get in there and do it. But I think if you get in there and do it a couple of times and get a good feel for it, I don’t see why nurses or anybody couldn’t be trained on this.”
And about EEG tech jobs? “I think new devices like Zeto are actually making the job for the EEG technologist much easier,” he adds. “Yes, other people can use it – I’m not a registered EEG tech, but I can use it effectively. But for an EEG tech, how much easier would their life be? Not having to measure, not having to use collodion, not having to scrub every spot.”
The implications extend beyond EEGs. As healthcare becomes increasingly specialized while rural hospitals face ongoing staffing challenges, technology that makes specialized procedures accessible to broader clinical teams becomes not just helpful, but essential.
“It all boils down to patient care,” Daniel emphasizes. “You want to make it as easy and as useful and as effective for the patient as possible. We want to make sure these patients are okay and they’re getting EEGs when they need it.”
To date, Western Reserve Hospital has performed approximately 120 EEGs using Zeto technology, managed entirely by Daniel Rhoades during his day shift. The hospital serves rural Ohio communities where specialized neurological services are often hours away.