Huntsville Memorial Hospital Reduces Patient Transfers and Enhances Local Care with Onsite EEG Program

How One Rural Hospital Reclaimed EEG Access
Every week, someone at Huntsville Memorial Hospital (HMH) used to make the same difficult call: “We need to transfer this patient out for an EEG.” For families already stretched thin by work, school, and everyday life in rural Texas, that meant a 30-mile drive – often at odd hours – to the nearest neuro center. By early 2025, HMH’s new Chief Medical Officer and a cross‑departmental task force realized these transfers weren’t just inconvenient; they were a barrier to timely care.

Turning Transfers into Local Admissions
Like many small rural hospitals in the United States, Huntsville Memorial Hospital (HMH) didn’t have EEG services. There were no local neurologists available to read the studies and no EEG techs on staff to perform them. So when a patient in the emergency room needed an EEG, the only option was to transfer them to a larger and higher-level facility with the necessary diagnostic tools. After reviewing two years of ED transfer data, hospital leadership found that nearly half of their neuro-related transfers – about ten patients a month – were happening solely because they couldn’t perform an EEG onsite.
“We dug into two years of ER transfer logs and half of those transfers were for some sort of neurological reasons,” says Joe Schorre, Director of Cardiopulmonary and Emergency Management. “Of those, about 10 patients a month we felt could admit instead of shipping out if we had onsite EEG capabilities.”
That insight sparked a bold aim: bring EEG testing back onsite. Until 2015, HMH had in‑house EEG capability; for the past decade, any hint of seizure work‑up triggered an out of hospital transfer. The task force set out to reverse that trend.
Selecting the Right Technology
“If I Can Get a Full EEG for the Same Price, Why Wouldn’t I?”
When Huntsville Memorial began evaluating EEG solutions, ease of use and clinical quality were top priorities. As someone without a background in EEG, Joe Schorre wanted a system he and his team could easily understand and operate – something simple enough to support, but robust enough to meet physicians’ expectations. Many rapid EEG options offered just 8 to 12 channels, but Zeto ONE system delivered a full EEG without gels or pastes. “If I can get a full EEG for the same price as a limited one, why wouldn’t I?” he said. The combination of full diagnostic capability, ease of use, and pricing made Zeto the clear choice.

From Pilot to Practice
“If I Expect My Staff to Do It Right, I Have to Train Them Right”
For Joe Schorre, the success of Huntsville Memorial’s EEG program hinged not just on picking the right technology—but on implementing it the right way. “If I expect my staff to do it correctly, I need to make sure they’re trained correctly,” he said. That mindset shaped every step of the rollout. The hospital’s respiratory therapists, who were already stretched thin responding to codes and covering other clinical duties, were given protected time to train—without distractions or overlapping responsibilities. “We blocked out time so they weren’t trying to answer phones or get pulled away,” Joe explained. “They could just focus on learning.”
Joe and his team developed a step-by-step workflow for setup and procedure, making sure it was something staff could rely on in real clinical settings. “This was something they’d never done before, so we had to give them the resources to feel confident,” he said.
Clear communication with the hospital team was also a critical part of Huntsville Memorial Hospital’s EEG program rollout.
“We worked with our medical staff to make sure they understood – my team are not EEG technicians,” said Schorre. “They don’t know how to identify a seizure during the test.”
“We do utilize the NeuroPulse AI – Status Epilepticus and Seizure Burden bedside software from Zeto and encevis’ as a trigger,” Joe explained. “If the seizure burden crosses a threshold we set, a routine exam is automatically upgraded to STAT, triggering an alert to the epileptologist, who logs in, confirms the seizure activity, and contacts the ordering provider with recommendations.”
The staff felt comfortable with what we’re doing because from the start, they were trained, supported, and set up for success.
How Teleneurology Service Works at HMH
As part of a broader initiative, Huntsville Memorial Hospital expanded both its stroke program and inpatient teleneurology services. EEGs are interpreted entirely by remote neurology partners Blue Sky Telehealth (CarePoint), and staff are only contacted if there’s a technical issue. “The only time my staff are contacted by the teleneurology service is if there’s a technical issue they notice,” said Joe Schorre. “They’ll call our staff and ask them to redo it – but that’s only happened once.” The workflow is streamlined, with clearly defined roles and strong communication.
Since launching the program with Zeto in December 2024, HMH has generated at least 40 admissions that would have previously required transfers. Before, even the suspicion that an EEG might be needed meant transferring the patient. Now, with onsite EEG and inpatient teleneurology, those patients can stay and be treated locally.
Zeto ONE Cleaning Protocol: “Five Minutes and Done”
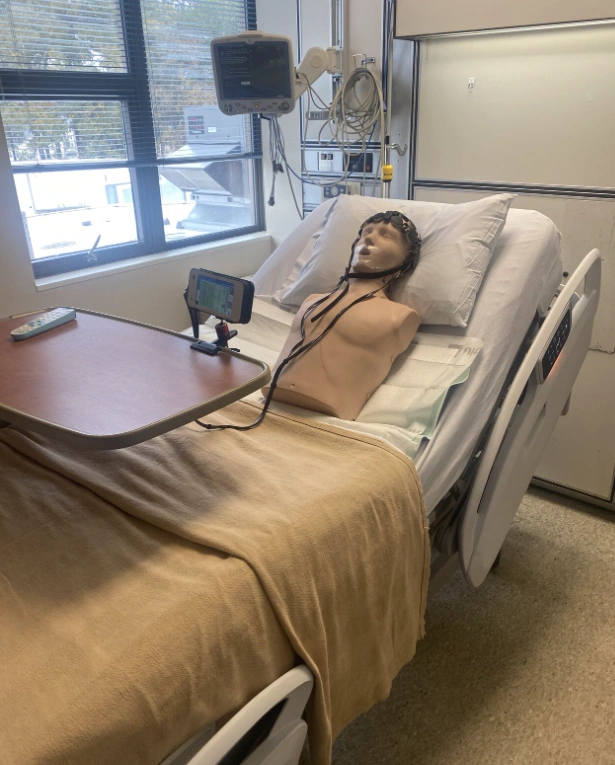
EEG headsets are stored in protective cases in a designated workroom near the testing area. The EEG display units are kept upright in a desk organizer and plugged in for charging, ready for the next use.
After each EEG, staff use SaniWipes (hospital-approved germicidal disposable wipes) to disinfect the headset. “We haven’t had any issues,” said Joe. “It takes maybe five minutes, and our infection control team has been satisfied with the process.”
Launching an Outpatient EEG Service
Huntsville Memorial has also launched an outpatient EEG program designed to give referring physicians faster, easier access to essential diagnostic data.
“One of the things that our primary care doctors are very excited about is having the ability to refer a patient to us for EEG testing,” said Joe Schorre. The goal is to allow patients to complete their EEG – and MRI – locally, before being referred to a specialist “down south,” where most of the region’s neurologists are located. When patients finally arrive at their neurology appointments – often after months of waiting – they now have their EEGs in hand to move care forward without delay. To simplify referrals, Joe even created an outpatient referral form for local primary care providers with the most common ICD-10 codes for EEG orders.
To make outpatient testing financially sustainable, HMH turned to Zeto’s different product, WR19 EEG headset – well-suited for routine EEGs in outpatient settings. While the Zeto ONE offers advanced features ideal for emergency and critical care, it wasn’t a viable choice for outpatient use given the state’s Medicare reimbursement rate of just $336 per EEG.
Launching the outpatient EEG program is more than a matter of convenience – it’s a strategic step toward addressing systemic access issues and closing gaps in rural care. “We’re the old-school county hospital,” Joe said. “We’re not part of a large health system – we’re the only hospital in town.” For many patients, traveling to Conroe, The Woodlands, or the Houston Medical Center simply isn’t possible. Now, they can complete critical testing locally, avoid unnecessary delays, and in some cases, begin treatment sooner.
–
With both inpatient and outpatient programs now in place, the hospital has not only reduced avoidable transfers but also strengthened its ability to provide timely, local care across the community. From patients in the ER to those referred by primary care more people in the Huntsville area can now receive neurological evaluation without the disruption of travel. What started as an effort to solve a transfer problem has evolved into a model for rural hospitals aiming to close critical care gaps with the help of the right tools, partners, and training.
About Huntsville Memorial Hospital
Huntsville Memorial Hospital, Huntsville, Texas, is currently a 123-bed, CIHQ‐accredited, not‐for‐profit acute care community hospital. HMH delivers quality healthcare services to the residents of Walker County and its surrounding communities, a population of more than 82,000. HMH and its dedicated staff offer compassionate care and the latest technologies and treatment solutions. HMH holds the American Heart Association Primary Stroke Center designation. HMH keeps community health and wellness at the forefront of its mission.


